Acid Reflux / GORD
Welcome to Qoctor’s online doctor service which can provide assessment for GORD/Acid Reflux. Answer some online questions, then book a video consultation with an AHPRA-registered doctor. Repeats available.
The consultation fee is $29.99. If a prescription is advised, it can be sent as an eScript to your phone OR electronically to your local pharmacy. Alternatively you can have medication delivered by an Australian partner pharmacy- in this case, the cost of medication is added at the checkout. All treatment and advice is issued subject to your consultation and the doctor’s assessment.
About Acid Reflux & GORD
- Gastro-oesophageal reflux disease (also known as GORD or acid reflux) is a common condition caused by acid rising from the stomach into the oesophagus (food pipe). This can cause symptoms such as heartburn, nausea, bloating, indigestion, belching, a taste of acid in the mouth, and sometimes a dry cough.
- It can be triggered by various things, such as acidic or rich foods, large meals, alcohol, being overweight, and smoking.
- If you’ve had reflux for a few days, a short course of antacid medication may get rid of the symptoms. If this does not work, it’s essential you see a doctor for a check up, as there can be a more serious underlying condition.
- Some people suffer from reflux on an ongoing basis and need to take antacids every day. Anyone who needs long term antacids should have a camera test (gastroscopy) to make sure there is nothing more serious going on, and should also have a check up with their doctor every 6 to 12 months.

Common Questions and Answers
Gastro-oesophageal reflux disease (GORD) is a general term which encompasses acid reflux, heartburn, indigestion and oesophagitis. It may include one or more of these conditions. It is caused by irritation of the stomach or food pipe (oesophagus) by stomach acid.
The stomach naturally makes acid as part of the normal digestion process. Usually the sphincter at the bottom of the oesophagus acts as a valve and keeps this acid in the stomach. Acid reflux can happen if this sphincter is weak, if there is too much acid made in the stomach, if the stomach is not emptying properly, or if there is increased pressure in the stomach, forcing acid back up into the oesophagus.
Many things can trigger Acid Reflux / GORD including:
- Smoking
- Caffeine
- Alcohol
- Hiatus Hernia
- Helicobacter Pylori ( a common infection of the stomach)
- Acidic or spicy food and drink
- Large fatty meals
- Obesity
- Stress
- Pregnancy
- Medications (including anti-inflammatories, certain blood pressure medications, sleeping tablets and painkillers)
The main symptom of GORD is heartburn. This is a discomfort or burning sensation which rises from the upper tummy or lower chest up towards the neck. Other common symptoms include:
- Nausea
- Belching
- Indigestion
- An acid-like taste in the mouth
- Persistent dry cough
- A feeling of a lump in the throat
- A burning pain when you swallow hot drinks
Symptoms tend to be worse after or with meals.
If you get any of the following symptoms you should seek immediate medical attention. They may indicate a more serious underlying condition:
- Chest pain or upper tummy pain worse on exertion
- Difficulty swallowing foods or liquids
- Persistent pain on swallowing
- Persistent vomiting
- Vomiting blood or dark brown vomit
- Unexplained weight loss
- Altered bowel habit (diarrhoea or constipation) for more than 6 weeks
- Altered stool (dark or black poo)
- Lump in the abdomen (tummy)
- Unexplained anaemia
- Jaundice
- New GORD symptoms in someone aged 55 years or over
- GORD symptoms with any of the following:
- Family history of stomach or oesophageal cancer in more than two first degree relatives
- Barrett’s oesophagus
- Pernicious anaemia
- Previous stomach ulcer surgery
- Pernicious anaemia
- A previous diagnosis of the following stomach conditions: dysplasia, atrophic gastritis or intestinal metaplasia
Most people are diagnosed with GORD by their GP on the basis of their typical symptoms and their response to treatment. Further tests may be needed if:
- Symptoms are severe
- Do not improve with treatment
- Are not typical of GORD
- There are any red flag symptoms
If further investigation is required a gastroscopy is usually the next step. This is where a thin, flexible telescope is passed down the oesophagus into the stomach. A normal test helps to rule out more serious causes of reflux symptoms, particularly stomach cancer.
Lifestyle changes may help, such as and avoid triggers- for example avoiding smoking, alcohol and weight gain. There are over the counter medications which help to neutralise acid, as well as other medications which may be prescribed by doctors, subject to assessment.
Oesophageal stricture– Acid Reflux / GORD can cause scarring and narrowing of the food pipe called an oesophageal stricture if left untreated. This can lead to difficulty swallowing, and problems eating and drinking.
Barrett’s oesophagus – this is a complication of long standing, untreated Acid Reflux / GORD. The excess acid causes a permanent change in the cells that line the oesophagus. It increases the risk of developing cancer of the oesophagus, and thus needs to be managed and monitored.
But most people with Acid Reflux / GORD do not develop any of these complications. If you have any concerns then you should discuss them with your doctor.
Health Library- Digestion & Bowel Health
Haemorrhoids
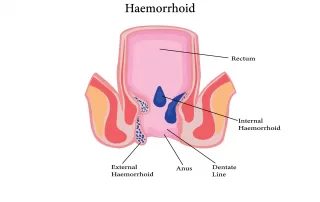
Haemorrhoids Haemorrhoids, also known as piles, are a very common medical condition. The pelvis and anus have a lot of blood vessels, and around the rectum, some veins are very close to the skin. This means if they pool with blood and enlarge, they can become prominent and present as haemorrhoids. Haemorrhoids can occur at any age and studies around the world report anywhere between 5-50% of the population experiencing them at some point in their lives. Book a GP appointment Symptoms of haemorrhoids Haemorrhoids can be internal or external. Internal means they are inside the rectal canal and aren’t often visible unless they prolapse out of the anus. External ones can be anywhere between 2cm inside the rectum to the skin of the anus, so they may or may not be visible. Generally speaking, internal [...]
Ulcerative colitis
Ulcerative colitis Ulcerative colitis (UC) is a condition where inflammation occurs in the large bowel (colon) and the rectum. It is one of two major inflammatory bowel diseases, the other being Crohn’s disease which can affect the whole gastrointestinal tract from the mouth to the anus. UC is about three times more common than Crohn’s disease and affects approximately 1-5 people in 1,000. It is slightly more common in women than men and the peak incidence occurs between 18 and 40. Book a GP appointment Causes and risk factors The cause is unknown, but it is thought to be an autoimmune condition which means the body attacks the bowel. Some associations with UC include: Family history of UC or Crohn’s disease Medications, such as anti-inflammatories and antibiotics Infections, such as gastroenteritis caused by bacteria or viruses [...]
How to get rid of acid reflux
Acid reflux- causes and treatment Acid reflux is when stomach acid flows from the stomach upwards into the oesophagus. The oesophagus (us-off-a-gus) is the tube connecting your mouth with your stomach. Acid reflux can cause irritation of the lining of the oesophagus. Gastro-oesophageal reflux disease (GORD or GERD) may be present if someone has symptoms of acid reflux more than twice a week. Many people experience acid reflux from time to time. While most people can manage the symptoms with lifestyle changes and simple medications from their pharmacy, some people suffering from GORD may need stronger medications or even surgery to treat their symptoms. Anyone with acid reflux or GORD symptoms that are not settling, or that are getting worse over time, should seek medical advice, as investigations may be required to rule out more serious underlying conditions. Symptoms The main symptom of [...]